WHAT IS PLATELET RICH PLASMA (PRP)?
PRP is derived from whole blood and contains:
1. A small amount of plasma
2. A high concentration of platelets
(up to a 8-10 fold increase relative to whole blood)
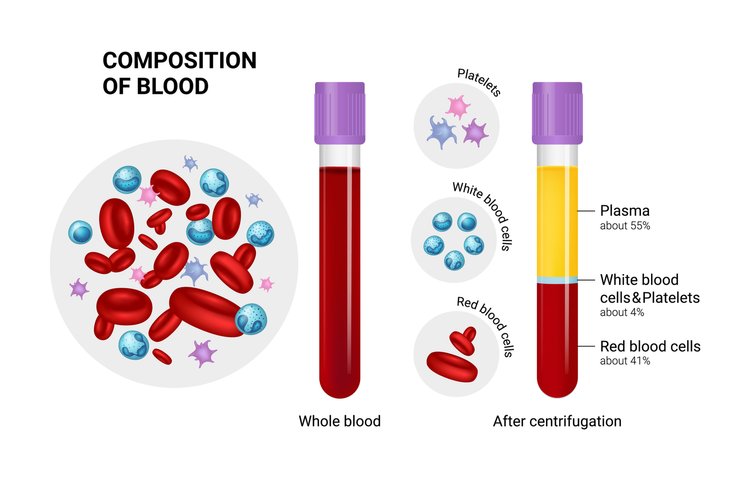
Whole blood is composed of:
1. 55% plasma
2. 41% red blood cells
3. 4% white blood cells and platelets
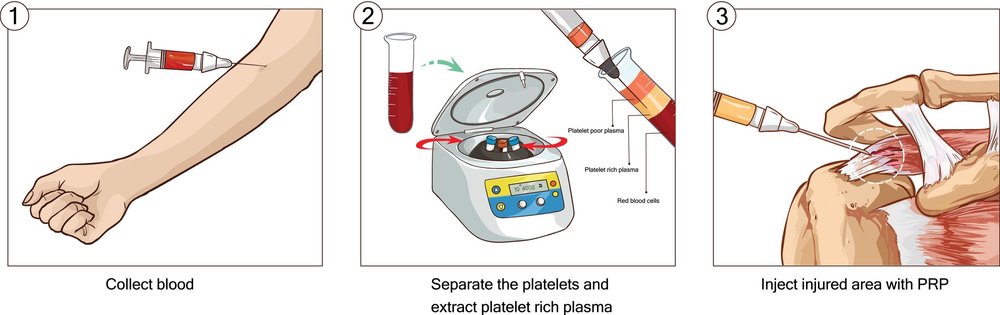
PRP is derived when an individual’s whole blood (25 – 180 mL) is drawn and put into a centrifuge to separate the red blood cells and excess plasma, with an end product of plasma rich in platelets (2 to 5 mL). Once separated, the PRP is injected into the injured area to accelerate tissue repair and regeneration.
HOW DOES PRP ACCELERATE HEALING?
When an injury occurs, the human body naturally recruits platelets and other blood cells to heal the damage. Platelets are a primary cell type present during the acute phase of an injury and act to initiate wound healing. Although platelets are most commonly known for their ability to form a clot and stop bleeding, they are responsible for:
1. Bringing white blood cells to the injured area to help resolve chronic, stagnant swelling.
2. Secreting growth factors that are directly responsible for tissue regeneration and wound healing.
3. Increasing chondrocytes, the cells which grow into cartilage tissue.
4. Signalling and recruiting mesenchymal stem cells and fibroblasts, the cells that produce collagen.
Because PRP is so concentrated, it acts as a potent tissue growth stimulant and amplifies the natural process of tissue repair and regeneration to heal and strengthen the previously damaged area.
THERAPEUTIC HISTORY OF PRP
Doctors began performing PRP injections in the 1970’s to help very ill patients. It wasn’t until the 1990’s when PRP was used for musculoskeletal pain.
INDICATIONS
All joint, ligament, muscle and tendon areas can be treated, whether chronic or acute.
Achilles tendonitis Osteoarthritis Shoulder dislocations
Chronic low back pain Plantar fasciitis Tennis elbow
Meniscal tears Rotator cuff tears Whip lash, neck pain
FREQUENCY OF TREATMENTS
While responses to treatment vary, most people will require 2 to 6 sets of PRP injections spaced 6 to 12 weeks apart.
RISKS AND SIDE EFFECTS
PRP therapy is a relatively low-risk procedure. Soreness and/or bruising at the injection site are the most common side effects. More serious side effects are rare but may include:
- Light-headedness, fainting, myoclonus
- Infection
- Allergic reaction
- Nerve injuries
- Spinal headache
- Pneumothorax (collapsed lung) if injections are within proximity of the lungs
WHOE IS NOT A GOOD CANDIDATE FOR PRP THERAPY?
PRP is absolutely not recommended if:
- Same day airline travel
- Total replacement of the injured site (e.g., knee replacement as a synthetic joint cannot be regenerated)
PRP may not be recommended if:
- Surgical hardware (e.g., screws, anchors)
- Compromised circulation (e.g., in the presence of diabetes, cardiovascular disease)
- Cancer at or near the site
- Pregnant
- Smoker
- On immune suppressant drugs (e.g., prednisone, Imuran, methotrexate)
- Hormone deficiencies
TREATMENT COURSE
- Prehab (before treatment): Optimize the overall state of the body via adequate sleep, hydration, nutrition, and exercise prior to your visit. In PRP you’re literally using your own blood as the initial healing agent and the outcome can be influenced by your current health status.
- Blood draw: On the day of your appointment, the practitioner will draw 25 to 180 mL of your blood (note that 500 mL is taken in blood bank donations). Ensure you’re hydrated and have eaten beforehand to prevent feeling lightheaded.
- Blood processing: Once the blood is drawn, it will be placed into a centrifuge to extract the PRP. This will take 5 to 30 minutes.
- Injection: The PRP will then be injected into the site of injury.
- Rehab (after treatment): Proper management and care is essential to promote the best results:
- Limit or avoid any aggravating factors, if possible, and always remember that “pain is a request for change.”
- Continue other therapies that are supportive to healing (e.g., acupuncture, physiotherapy).
- Repeat: PRP is typically repeated 2 to 6 times about 1.5 to 3 months apart.
Note: Refer to my blog ‘PRE- & POST-INJECTION CARE’ to see how you can optimize your healing response.
HOW DOES PRP THERAPY COMPARE TO OTHER TREATMENT OPTIONS?
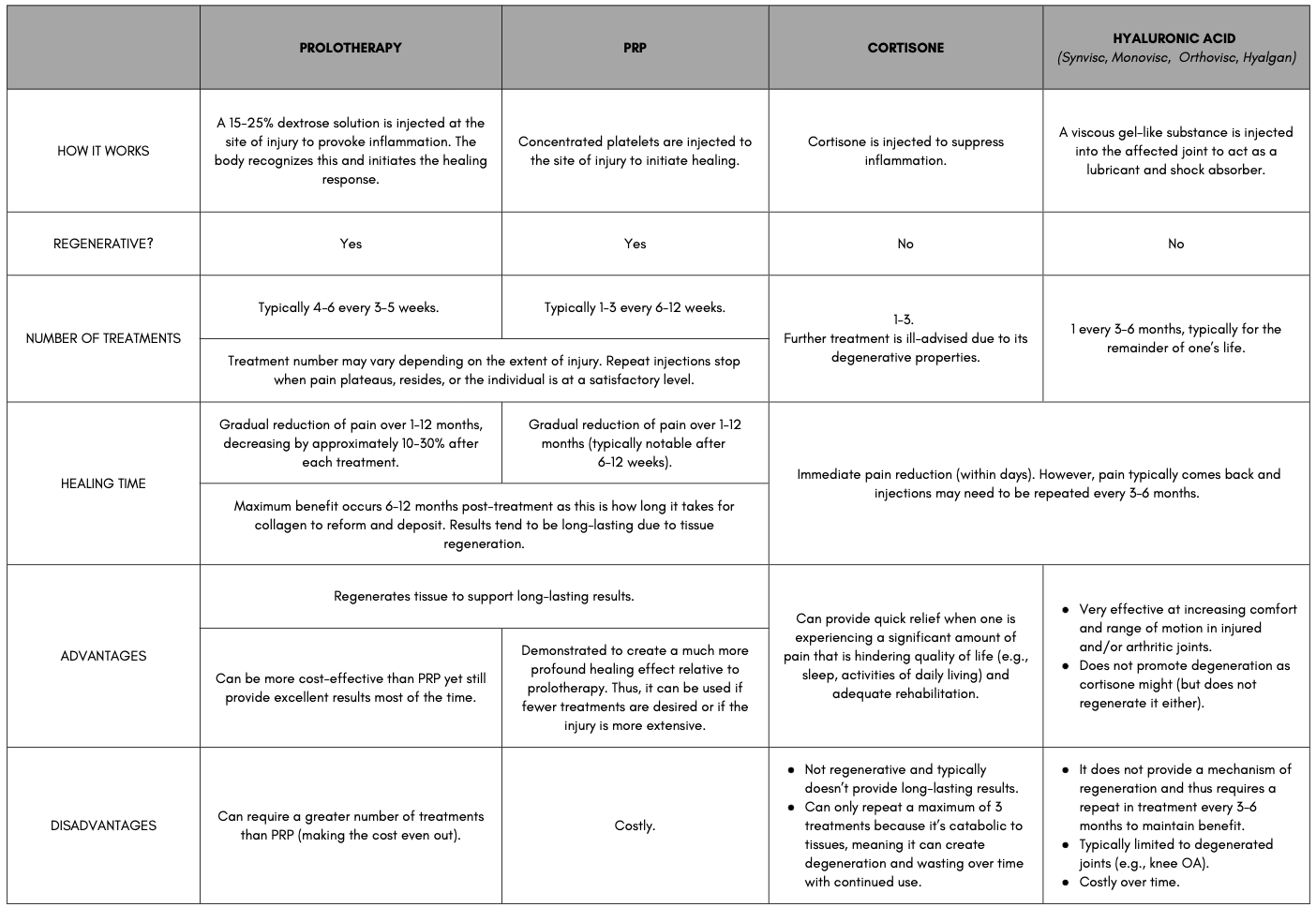
WHEN TO CONSIDER PRP AS YOUR BEST OPTION FOR REGENERATIVE INJECTION THERAPY
- Dextrose prolotherapy has resulted in some benefit with confidence the treatment has been performed properly but the results are not optimal.
- Severe, advanced, or complex injury.
- Labral or meniscal tears.
- Muscular tears.
- High performance athletes who place increased demand on joints.
- Persons who wish to maximize their results with a minimum number of injection visits (e.g., live out of town and cannot return frequently, needle phobia with a preference for less visits and fewer injections overall).
PROFESSIONAL SUCCESS STORIES
- Tiger Woods received PRP in his lateral collateral ligament (LCL) following a slow post-operative recovery from an ACL repair. VIDEO: Tiger Woods Admits Federal Investigators Have Contacted His Agent In Drug Probe (radaronline.com)
- World champion figure skater Patrick Chan received PRP to hasten the recovery of his calf. http://www.thestar.com/printarticle/712714 (drhalbrown.com); G&M (drhalbrown.com)
- Pittsburgh Steelers stars Hines Ward and Troy Polamalu received treatment prior to winning the Super Bowl. prpCTV (drhalbrown.com); G&M (drhalbrown.com)
- The major league baseball pitcher Takashi Saito received PRP for his strained elbow and regained his career. Takashi Saito (drhalbrown.com)
- Astros pitcher Doug Brocail received PRP for a hamstring injury. brocail (drhalbrown.com)
CLICK HERE TO WATCH AN INFORMATIONAL VIDEO!
RESEARCH SUMMARIES
PLANTAR FASCITIS
Tiwari, M., & Bhargava, R. (2013). Platelet rich plasma therapy: A comparative effective therapy with promising results in plantar fasciitis. Journal of Clinical Orthopaedics and Trauma, 4(1), 31-35. doi:10.1016/j.jcot.2013.01.008
- Treatment: Platelet Rich Plasma (5 mL) vs Steroid (40 mg methyl prednisolone acetate)
- Frequency: Single injection
- Participants: 60 participants; ages 30-85
This prospective two-arm non-blinded RCT compared platelet rich plasma (PRP) with steroid injection to compare the effects on plantar fasciitis. It was hypothesized that PRP injection would be superior to local steroid injection. Sixty participants, age 30 to 85 years, with medial tubercle calcaneum pain and tenderness upon weight bearing after rest were equally randomized to a single injection of platelet rich plasma or methyl prednisolone acetate. Outcome measurements were assessed the using the Visual Analog Scale (VAS) scale where a score of 0 is no pain and 10 is maximum pain. At one, three, and six months the VAS score was significantly improved in the PRP group, demonstrating superiority with this method in comparison to the steroid group. There were no complications in either group.
REFERENCES
- Abate, M., Di Carlo, L., & Salini, V. (2019). Platelet rich plasma compared to dry needling in the treatment of non-insertional achilles tendinopathy. The Physician and Sports Medicine, 47(2), 232-237. https://doi.org/10.1080/00913847.2018.1548886
- Agathocleous, M., Meacham, C,. Burgess, R. et al. (2017). Ascorbate regulates hematopoietic stem cell function and leukaemogenesis. Nature, 549, 476-481. https://doi.org/10.1038/nature23876
- Alderman, D. (2007). Prolotherapy for low back pain: A reasonable and conservative approach to MSK low back pain, disc disease, and sciatica. Retrieved from https://www.bowlermedical.org/uploads/3/9/3/5/39351519/low_back_prolo_case_studies.pdf
- Alves, R., Grimalt, R. (2018; 2017). A review of platelet-rich plasma: History, biology, mechanism of action, and classification. Skin Appendage Disorders, 4(1), 18-24. https://doi.org/10.1159/000477353
- Andia, I., Rubio-Azpeitia, E., & Maffulli, N. (2015). Platelet-rich plasma modulates the secretion of Inflammatory/Angiogenic proteins by inflamed tenocytes. Clinical Orthopaedics and Related Research, 473(5), 1624-1634. https://doi.org/10.1007/s11999-015-4179-z
- Bradley, J. P., Lawyer, T. J., Ruef, S., Towers, J. D., & Arner, J. W. (2020). Platelet-rich plasma shortens return to play in national football league players with acute hamstring injuries. Orthopaedic Journal of Sports Medicine, 8(4), 2325967120911731-2325967120911731. https://doi.org/10.1177/2325967120911731
- Brown, Hal (2015, October 29). Running injuries & rit: relief from chronic pain. Retrieved from https://ndnr.com/mens-health/running-injuries-rit-relief-from-chronic-pain/
- Cabezas-Wallscheid, N., Buettner, F., Sommerkamp, P., Klimmeck, D., Ladel, L., Thalheimer, F. B., et al (2017). Vitamin A-retinoic acid signaling regulates hematopoietic stem cell dormancy. Cell, 169(5), 807-823. https://doi.org/10.1016/j.cell.2017.04.018
- Ciftci, H., Yeni, E., Demir, M., Yagmur, I., Gümüş, K., Celik, H., Savas, M., & Gulum, M. (2013). Can the mean platelet volume be a risk factor for vasculogenic erectile dysfunction? The World Journal of Men’s Health, 31(3), 215-219. https://doi.org/10.5534/wjmh.2013.31.3.215
- Cortes, M., Chen, M., Stachura, D., Liu, S., Kwan, W., Wright, F., Vo, L., Theodore, L., Esain, V., Frost, I., Schlaeger, T., Goessling, W., Daley, G., & North, T. (2016). Developmental vitamin D availability impacts hematopoietic stem cell production. Cell Reports (Cambridge), 17(2), 458-468. https://doi.org/10.1016/j.celrep.2016.09.012
- Danieli, M. V., Pereira, H. d. R., Carneiro, Carlos Augusto de Sá, Felisbino, S. L., & Deffune, E. (2014). Treatment of osteochondral injuries with platelet gel. Clinics (São Paulo, Brazil), 69(10), 694-698. https://doi.org/10.6061/clinics/2014(10)08
- Deal, J. B., Smith, E., Heard, W., O’Brien, M. J., & Savoie, F. H. (2017). Platelet-rich plasma for primary treatment of partial ulnar collateral ligament tears: MRI correlation with results. Orthopaedic Journal of Sports Medicine, 5(11), 2325967117738238-2325967117738238. https://doi.org/10.1177/2325967117738238
- Fitzpatrick, J,. Bulsara, M. K., O’Donnel, J., & Zheng, M. H. (2019). Leucocyte-rich platelet-rich plasma treatment of gluteus medius and minimus tendinopathy: a double-blind randomization controlled trial with 2-year follow-up. The American Journal of Sports Medicine, 47(5). 1130-1137. https://doi.org/10.1177/0363546519826969
- Fonken, L. K., Aubrecht, T. G., Melendez-Fernandez, O. H., Weil, Z. M., & Nelson, R. J., (2013). Dim light and night disrupts molecular circadian rhythms and increases body weight. Journal of Biological Rhythems. 28(4), 262-271. https://doi.org/10.1177/0748730413493862
- Gasparvan, A. Y., Ayvazyan, L., Mikhailidis, D. P., & Kitas, G. D. (2001). Mean platelet volume: a link between thrombosis and inflammation? Current Phamarceutical Design, 17(1), 47-58. https://doi.org/10.2174/138161211795049804
- Haker, E., Egekvist, H., & Bjerring, P. (2000). Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjections. Journal of the Autonomic Nervous System, 79(1), 52-59. https://doi.org/10.1016/s0165-1838(99)00090-9
- Halpern, B., Chaudhury, S., Rodeo, S. A., Hayter, C., Bogner, E., Potter, H. G., & Nguyen, J. (2013). Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. Clinical Journal of Sport Medicine, 23(3), 238-239. https://doi.org/10.1097/JSM.0b013e31827c3846
- Han, C., Na, Y., Zhu, Y., Kong, L., Eerdun, T., Yang, X., & Ren, Y. (2019). Is platelet-rich plasma an ideal biomaterial for arthroscopic rotator cuff repair? A systematic review and meta-analysis of randomized controlled trials. Journal of Orthopaedic Surgery and Research, 14(1), 183-183. https://doi.org/10.1186/s13018-019-1207-9
- Harrison, T. E., Bowler, J., Levins, T. N., Cheng, A., & Reeves, K. D. (2020). Platelet yield and yield consistency for six single-spin methods of platelet rich plasma preparation. Platelets (Edinburgh), 31(5), 661-666. 661-666. https://doi.org/10.1080/09537104.2019.1663808
- Harrison, T. E., Bowler, J., Levins, T. N., Cheng, A., & Reeves, K. D. (2020). Platelet-rich plasma centrifugation changes leukocyte ratios. Cureus (Palo Alto, CA), 13(4), e14470-e14470. https://doi.org/10.7759/cureus.14470
- Heber, S., & Volf, I. (2015). Effects of physical (in)activity on platelet function. BioMed Research International, 2015, 165078-11. https://doi.org/10.1155/2015/165078
- Heidt, T., Sager, H. B., Courties, G., Dutta, P., Iwamoto, Y., Zaltsman, A., von Zur Muhlen, C., Bode, C., Fricchione, G. L., Denninger, J., Lin, C. P., Vinegoni, C., Libby, P., Swirski, F. K., Weissleder, R., & Nahrendorf, M. (2014). Chronic variable stress activates hematopoietic stem cells. Nature Medicine, 20(7), 754-758. https://doi.org/10.1038/nm.3589
- Herdea, A., Struta, A., Derihaci, R. P., Ulici, A., Costache, A., Furtunescu, F., Toma, A., & Charkaoui, A. (2022). Efficiency of platelet-rich plasma therapy for healing sports injuries in young athletes. Experimental and Therapeutic Medicine, 23(3)https://doi.org/10.3892/etm.2022.11139
- Hicks, J. J., Li, H., Philippon, M. J., Hurwitz, S. R., Huard, J., & Hogan, M. V. (2016). Customized platelet-rich plasma for skeletal muscle injuries. Orthopaedic Journal of Sports Medicine, 4(7_suppl4), 2325967116. https://doi.org/10.1177/2325967116S00143
- Hubbard, G. P., Wolffram, S., Lovegrove, J. A., & Gibbins, J. M. (2004). Ingestion of quercetin inhibits platelet aggregation and essential components of the collagen‐stimulated platelet activation pathway in humans. Journal of Thrombosis and Haemostasis, 2(12), 2138-2145. https://doi.org/10.1111/j.1538-7836.2004.01067.x
- Iwamura, C., Bouladoux, N., Belkaid, Y., Sher, A., & Jankovic, D. (2017). Sensing of the microbiota by NOD1 in mesenchymal stromal cells regulates murine hematopoiesis. Blood, 129(2), 171–176. https://doi.org/10.1182/blood-2016-06-723742
- Johal, H., Khan, M., Yung, S. P., Dhillon, M. S., Fu, F. H., Bedi, A., & Bhandari, M. (2019). Impact of platelet-rich plasma use on pain in orthopaedic surgery: A systematic review and meta-analysis. SAGE Publications. https://doi.org/10.1177/1941738119834972
- Josefsdottir, K. S., Baldridge, M. T., Kadmon, C. S., & King, K. Y. (2017). Antibiotics impair murine hematopoiesis by depleting the intestinal microbiota. Blood, 129(6), 729–739. https://doi.org/10.1182/blood-2016-03-708594
- Joshi Jubert, N., Rodríguez, L., Reverté-Vinaixa, M. M., & Navarro, A. (2017). Platelet-rich plasma injections for advanced knee osteoarthritis: A prospective, randomized, double-blinded clinical trial. Orthopaedic Journal of Sports Medicine, 5(2), 2325967116689386-2325967116689386. https://doi.org/10.1177/2325967116689386
- Kaminski, R., Kulinski, K., Kozar-Kaminska, K., Wielgus, M., Langner, M., Wasko, M. K., Kowalczewski, J., & Pomianowski, S. (2018). A prospective, randomized, double-blind, parallel-group, placebo-controlled study evaluating meniscal healing, clinical outcomes, and safety in patients undergoing meniscal repair of unstable, complete vertical meniscal tears (bucket handle) augmented with platelet-rich plasma. BioMed Research International, 2018, 9315815-9. https://doi.org/10.1155/2018/9315815
- Kraeutler, M. J., Houck, D. A., Garabekyan, T., Miller, S. L., Dragoo, J. L., & Mei-Dan, O. (2021). Comparing intra-articular injections of leukocyte-poor platelet-rich plasma versus Low–Molecular weight hyaluronic acid for the treatment of symptomatic osteoarthritis of the hip: A double-blind, randomized pilot study. Orthopaedic Journal of Sports Medicine, 9(1), 2325967120969210-2325967120969210. https://doi.org/10.1177/2325967120969210
- Li, Y., Zhu, S., Zhang, Y., Liu, T., Su, L., Zhang, Q., & Luo, Y. (2018). High fat diet-induced obesity exacerbates hematopoiesis deficiency and cytopenia caused by 5-fluorouracil via peroxisome proliferator-activated receptor γ. Experimental hematology, 60, 30–39.e1. https://doi.org/10.1016/j.exphem.2017.12.013
- Luo, Y., Chen, G., Hannemann, N., Ipseiz, N., Krönke, G., Bäuerle, T., Munos, L., Wirtz, S., Schett, G., & Bozec, A. (2015). Microbiota from obese mice regulate hematopoietic stem cell differentiation by altering the bone niche. Cell Metabolism, 22(5), 886-894. https://doi.org/10.1016/j.cmet.2015.08.020
- Marshall, D. A., Liu, X., Barnabe, C., Yee, K., Faris, P. D., Barber, C., Mosher, D., Noseworthy, T., Werle, J., & Lix, L. (2019). Existing comorbidities in people with osteoarthritis: A retrospective analysis of a population-based cohort in alberta, canada. BMJ Open, 9(11), e033334-e033334. https://doi.org/10.1136/bmjopen-2019-033334
- Mascarenhas, R., Saltzman, B. M., Fortier, L. A., & Cole, B. J. (2015). Role of platelet-rich plasma in articular cartilage injury and disease. The Journal of Knee Surgery, 28(1), 003-010. https://doi.org/10.1055/s-0034-1384672
- Mills, F. B., Misra, A. K., Goyeneche, N., Hackel, J. G., Andrews, J. R., & Joyner, P. W. (2021). Return to play after platelet-rich plasma injection for elbow UCL injury: Outcomes based on injury severity. Orthopaedic Journal of Sports Medicine, 9(3), 2325967121991135-2325967121991135. https://doi.org/10.1177/2325967121991135
- Murphy, K. J., Chronopoulos, A. K., Singh, I., Francis, M. A., Moriarty, H., Pike, M. J., Turner, A. H., Mann, N. J., & Sinclair, A. J. (2003). Dietary flavanols and procyanidin oligomers from cocoa (theobroma cacao) inhibit platelet function. The American Journal of Clinical Nutrition, 77(6), 1466-1473. https://doi.org/10.1093/ajcn/77.6.1466
- Murphy, E. A., Davis, J. M., Carmichael, M. D., Gangemi, J. D., Ghaffar, A., & Mayer, E. P. (2008). Exercise stress increases susceptibility to influenza infection. Brain, Behavior, And Immunity, 22(8), 1152–1155. https://doi.org/10.1016/j.bbi.2008.06.004
- Nahrendorf, M., & Swirski, F. K. (2015). Lifestyle effects on hematopoiesis and atherosclerosis. Circulation Research, 116(5), 884-894. https://doi.org/10.1161/CIRCRESAHA.116.303550
- Oliveira, D. C., Nogueira-Pedro, A., Santos, E. W., Hastreiter, A., Silva, G. B., Borelli, P., & Fock, R. A. (2018). A review of select minerals influencing the haematopoietic process. Nutrition Research Reviews, 31(2), 267–280. https://doi.org/10.1017/S0954422418000112
- Ozdemir, O., Soylu, M., Alyan, O., Geyik, B., Demir, A. D., Aras, D., Cihan, G., Cagirci, G., Kacmaz, F., Balbay, Y., Sasmaz, H., & Korkmaz, S. (2004). Association between mean platelet volume and autonomic nervous system functions: Increased mean platelet volume reflects sympathetic overactivity. Experimental and Clinical Cardiology, 9(4), 243-247.
- Pan, P., Wang, J., Tsai, C., & Kuo, H. (2022). Identification of early response to hypertonic dextrose prolotherapy markers in knee osteoarthritis patients by an inflammation-related cytokine array. Journal of the Chinese Medical Association, 85(4), 525-531. https://doi.org/10.1097/JCMA.0000000000000693
- Park, P. Y. S., Cai, C., Bawa, P., & Kumaravel, M. (2018;2019;). Platelet-rich plasma vs. steroid injections for hamstring injury—is there really a choice? Skeletal Radiology, 48(4), 577-582. https://doi.org/10.1007/s00256-018-3063-9
- Pauly, S., Klatte-Schulz, F., Stahnke, K., Scheibel, M., & Wildemann, B. (2018). The effect of autologous platelet rich plasma on tenocytes of the human rotator cuff. BMC Musculoskeletal Disorders, 19(1), 422-422. https://doi.org/10.1186/s12891-018-2339-5
- Prodromos, C. C., Finkle, S., Prodromos, A., Chen, J. L., Schwartz, A., & Wathen, L. (2021). Treatment of rotator cuff tears with platelet rich plasma: A prospective study with 2 year follow‐up. BMC Musculoskeletal Disorders, 22(1), 1-499. https://doi.org/10.1186/s12891-021-04288-4
- Ranjith, M. P., DivyaRaj, R., Mathew, D., George, B., & Krishnan, M. N. (2016). Mean platelet volume and cardiovascular outcomes in acute myocardial infarction. Heart Asia, 8(1), 16-20. https://doi.org/10.1136/heartasia-2015-010696
- Rosenwinkel, E. T., Bloomfield, D. M., Arwady, M. A., & Goldsmith, R. L. (2001). Exercise and autonomic function in health and cardiovascular disease. Cardiology Clinics, 19(3), 369–387. https://doi.org/10.1016/s0733-8651(05)70223-x
- Ruf J. C. (2004). Alcohol, wine and platelet function. Biological Research, 37(2), 209–215. https://doi.org/10.4067/s0716-97602004000200006
- Shahid, M., & Kundra, R. (2017). Platelet-rich plasma (PRP) for knee disorders. EFORT Open Reviews, 2(1), 28-34. https://doi.org/10.1302/2058-5241.2.160004
- Singer, K., DelProposto, J., Lee Morris, D., Zamarron, B., Mergian, T., Maley, N., Cho, K. W., Geletka, L., Subbaiah, P., Muir, L., Martinez-Santibanez, G., & Nien-Kai Lumeng, C. (2014). Diet-induced obesity promotes myelopoiesis in hematopoietic stem cells. Molecular Metabolism (Germany), 3(6), 664-675. https://doi.org/10.1016/j.molmet.2014.06.005
- Studzinski, G. P., Harrison, J. S., Wang, X., Sarkar, S., Kalia, V., & Danilenko, M. (2015). Vitamin D control of hematopoietic cell differentiation and leukemia: V ITAMIN D C ONTROL. Journal of Cellular Biochemistry, 116(8), 1500-1512. https://doi.org/10.1002/jcb.25104
- Swain, S., Sarmanova, A., Coupland, C., Doherty, M., & Zhang, W. (2020;2019;). Comorbidities in osteoarthritis: A systematic review and Meta‐Analysis of observational studies. Arthritis Care & Research (2010), 72(7), 991-1000. https://doi.org/10.1002/acr.24008
- Taya, Y., Ota, Y., Wilkinson, A. C., Kanazawa, A., Watarai, H., Kasai, M., Nakauchi, H., & Yamazaki, S. (2016). Depleting dietary valine permits nonmyeloablative mouse hematopoietic stem cell transplantation. Science (New York, N.Y.), 354(6316), 1152–1155.
- Thepsoparn, M., Thanphraisan, P., Tanpowpong, T., & Itthipanichpong, T. (2021). Comparison of a platelet-rich plasma injection and a conventional steroid injection for pain relief and functional improvement of partial supraspinatus tears. Orthopaedic Journal of Sports Medicine, 9(9), 23259671211024937-23259671211024937. https://doi.org/10.1177/23259671211024937
- Tischer, T., Bode, G., Buhs, M., Marquass, B., Nehrer, S., Vogt, S., Zinser, W., Angele, P., Spahn, G., Welsch, G. H., Niemeyer, P., & Madry, H. (2020). Platelet-rich plasma (PRP) as therapy for cartilage, tendon and muscle damage – german working group position statement. Journal of Experimental Orthopaedics, 7(1), 64-64. https://doi.org/10.1186/s40634-020-00282-2
- Trompette, A., Gollwitzer, E. S., Yadava, K., Sichelstiel, A. K., Sprenger, N., Ngom-Bru, C., Blanchard, C., Junt, T., Nicod, L. P., Harris, N. L., & Marsland, B. J. (2014). Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nature Medicine, 20(2), 159-166. https://doi.org/10.1038/nm.3444
- Uzun, H., Bitik, O., Uzun, Ö., Ersoy, U. S., & Aktaş, E. (2017). Platelet-rich plasma versus corticosteroid injections for carpal tunnel syndrome. Journal of Plastic Surgery and Hand Surgery, 51(5), 301-305. https://doi.org/10.1080/2000656X.2016.1260025
- Valacchi, G., & Bocci, V. (1999). Studies on the biological effects of ozone: 10. release of factors from ozonated human platelets. Mediators of Inflammation, 1999(4), 205-209. https://doi.org/10.1080/09629359990360
- van den Berg, S. M., Seijkens, T. T., Kusters, P. J., Beckers, L., den Toom, M., Smeets, E., Levels, J., de Winther, M. P., & Lutgens, E. (2016). Diet-induced obesity in mice diminishes hematopoietic stem and progenitor cells in the bone marrow. FASEB Journal : Official Publication Of The Federation Of American Societies For Experimental Biology, 30(5), 1779–1788. https://doi.org/10.1096/fj.201500175
- Xia, S., Li, X., Cheng, L., Han, M., Zhang, M., Shao, Q., Xu, H., & Qi, L. (2015). Fish Oil–Rich diet promotes hematopoiesis and alters hematopoietic niche. Endocrinology (Philadelphia), 156(8), 2821-2830. https://doi.org/10.1210/en.2015-1258
- Yoshida, M., & Marumo, K. (2019;2017;). An autologous leukocyte-reduced platelet-rich plasma therapy for chronic injury of the medial collateral ligament in the knee: A report of 3 successful cases. Clinical Journal of Sport Medicine, 29(1), e4-e6. https://doi.org/10.1097/JSM.0000000000000515
- Yu, T., Pang, J. S., Lin, L., Cheng, J., Liu, S., & Tsai, W. (2021). Platelet-rich plasma releasate promotes early healing in tendon after acute injury. Orthopaedic Journal of Sports Medicine, 9(4), 2325967121990377-2325967121990377. https://doi.org/10.1177/2325967121990377
- Zhang, J., Li, F., Augi, T., Williamson, K. M., Onishi, K., Hogan, M. V., Neal, M. D., & Wang, J. H. -. (2021). Platelet HMGB1 in platelet-rich plasma (PRP) promotes tendon wound healing. PloS One, 16(9), e0251166-e0251166. https://doi.org/10.1371/journal.pone.0251166